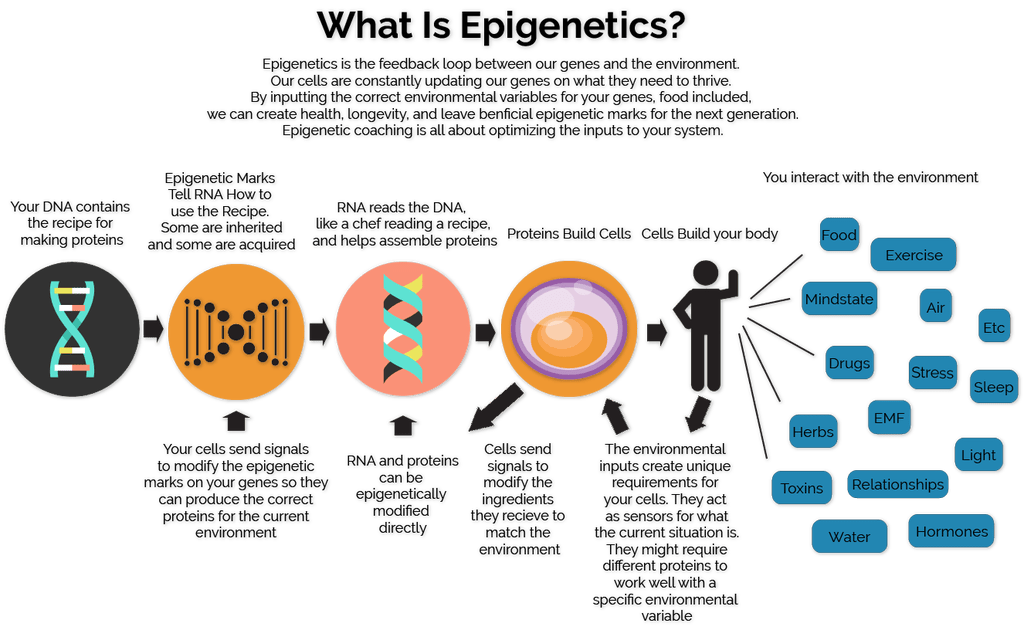
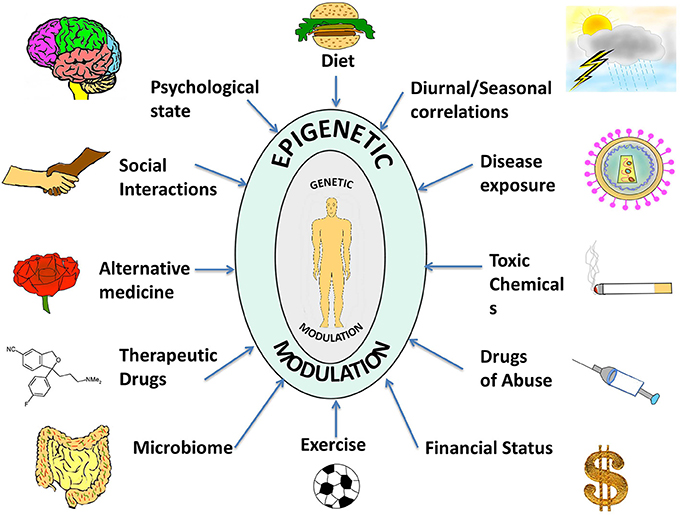
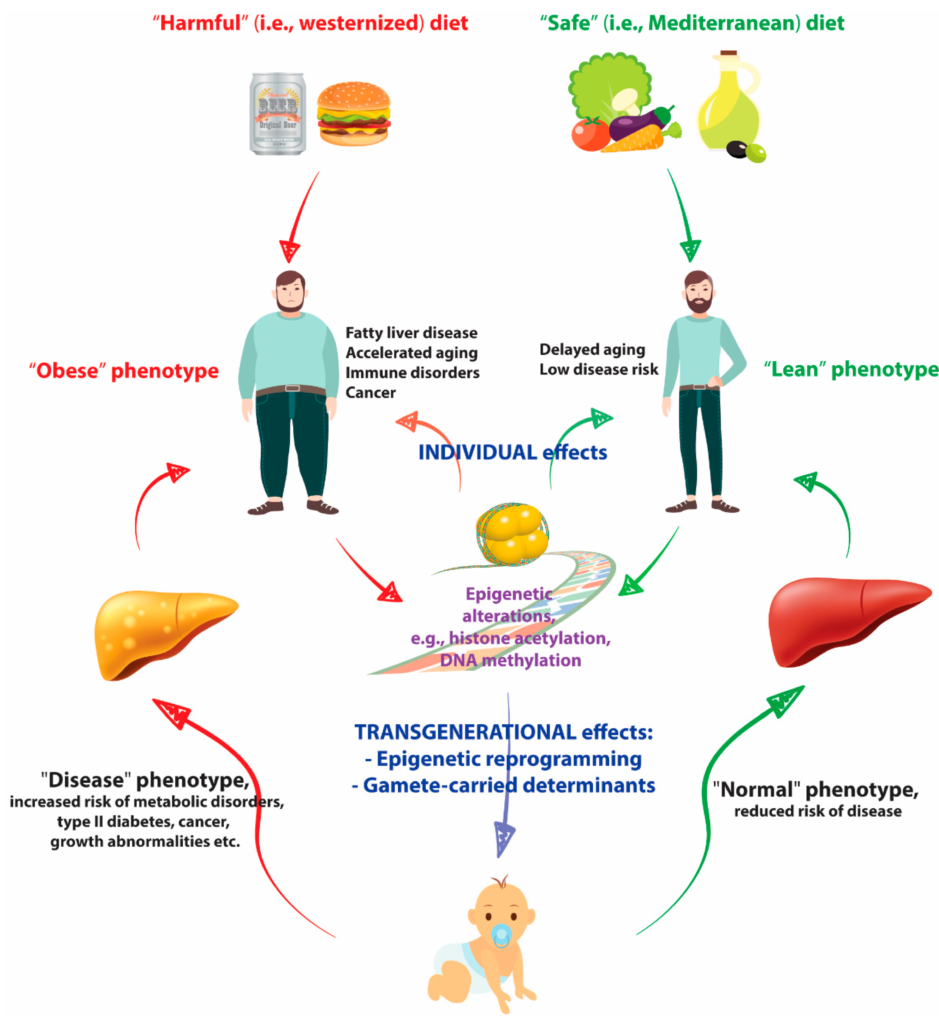
I am using the term epigenetics in it’s broadest sense here. The science of epigenetics refers to the controlling of gene expressions. Generally speaking, a gene is active when it is turned on and non-active when turned off, so it’s like a switch. The science explicitly associated with how the environment affects our gene expression is epigenetics, the science related to how our nutrition effects our gene expression is nutrigenomics.
Each of your 50 trillion to 60 trillion cells contains a complete set of Homo sapiens DNA instructions that are divided into subsets called genes. There are approximately 20,000 different genes located on the long strands of DNA in each cell. Assorted genes throughout your body are constantly working, orchestrating the building of critical protein structures and enzyme pathways, and repairing, regenerating, and sometimes even destroying your cells based on the signals they get from their immediate environment.
Genes are commonly viewed in a narrow dimension: the fixed heritable traits that we have little influence over, such as hair color, eye color, and predispositions toward specific personality characteristics or diseases. The impact of the
Coded into our familial genes are traits that the environment has little to no influence over, such as eye, hair, and skin color; facial features; body shape,
We all share the identical genetic code that makes us Homo sapiens. The code has been
While we are most certainly stuck with our eye and hair
Turn on “good” gene switches and you build muscle, increase fat burning, knock out an invading virus, or neutralize the oxidative damage to cells that characterizes the process of
While each human has a complex makeup of genes that is entirely unique, it’s important to understand that genes have no effect until they are expressed. The concept that genes have no effect until they are expressed is particularly relevant to those concerned with familial predispositions toward health problems, because conditions that are strongly associated with lifestyle (obesity, most cancers, heart disease, even arthritis,
Long-term health: The mission of your genes is to promote short-term survival through homeostasis, the synchronistic functioning of all systems in the body. Genes don’t know or care whether the signals you give them promote or compromise long-term health. They simply operate as they have been designed to do by evolution,
The development of type 2 diabetes, the exhaustion of the insulin-producing mechanism in the body to the extent that insulin injections become necessary to regulate blood sugar, is actually an example of the body doing what it is supposed to do over and over again until it finally becomes exhausted. Excess glucose in the bloodstream is toxic and can become life-threatening in a short time, so pumping out insulin after the consumption of thousands of sodas, cereal bowls, and energy bars over decades is the body’s valiant, and desirable, effort to ensure short-term survival.
Similarly, the stimulation of the fight-or-flight response is obviously a design feature that promotes short-term survival in the face of life-threatening circumstances by enhancing both physical and mental function. The very common abuse of the fight-or-flight response that occurs due to the unrelenting stress and stimulation of modern life is another example of mismanaging the gifts of our Homo sapiens genes and compromising long-term health. Furthermore, prescription drugs are designed to manipulate gene expression by overriding natural homeostatic mechanisms to act directly upon various genes associated with the condition being treated. This can generate dramatic short-term results, without accounting for the long-term adverse health implications.
We have a blueprint for healthy living embedded in our Homo sapiens genetic code the DNA that resides in every cell of our bodies. This blueprint was created through the magnificent process of human evolution. Our genes expect healthy foods; frequent movement; regular brief, intense strength,
Gene expression happens instantly in response to eating a certain meal, conducting a certain workout, or even thinking a certain positive or negative thought. Always, genes respond to
To promote long-term health, a pattern of living that promotes optimal gene expression (over both the short term and the long term) must be followed for approximately 21 days to solidify the process of gene reprogramming. For example, altering diet to moderate insulin production will up-regulate fat- and keto-burning genes and down-regulate glucose-burning genes. As this pattern is followed, excess body fat can be removed and kept off, daily energy levels regulated (instead of being dependent upon regular carbohydrate feedings), and disease risk factors normalized. Ceasing screen use after dark and increasing the duration of sleep each night for 21 days will normalize stress hormone levels and optimize immune and cognitive function throughout the day. Over the long term, this pattern will result in less afternoon or evening fatigue, fewer sugar cravings, more reliable evening release of melatonin, and subsequently more ease adhering to optimal sleeping habits.
The rapid effects of gene reprogramming can be observed by considering the blood markers for Metabolic Syndrome, the catch-all term that describes a litany of health problems relating to modern diet and lifestyle practices, most notably excess insulin production from a high-carbohydrate eating pattern. Metabolic Syndrome afflicts one in five Americans and is believed by many medical experts to represent today’s number one public health challenge. Physicians use five generally accepted markers for this condition: elevated fasting blood glucose, high blood pressure, excess waistline measurement, high triglycerides, and low HDL. Of the five, four can be manipulated into safe zones in as little as 21 days of diet and exercise modification. Excess body fat around the waistline can also be significantly improved with a little more time, perhaps a few more weeks or a few more months depending on one’s starting point. All the rapid changes in blood chemistry and body composition can be maintained long term through improved eating and lifestyle practices.
Systemic inflammation, or chronic inflammation, caused by long-term adverse lifestyle practices such as eating a high-carbohydrate diet, can result in undesirable gene expression and mutation. Inflammation is the body’s natural response to harmful environmental stimuli, such as a trauma or infection. The immune system’s inflammatory response is a critical component of health and homeostasis. However, this inflammatory response, like the fight-or-flight response, is designed to respond to acute stimuli, not chronic stressors. For example, when we sustain a bee sting, take an elbow to the face in a basketball game, or turn an ankle on a hiking trail, the inflammatory response of tissue swelling in the injured area helps your body quarantine the damage from the trauma to the affected areas. Without the acute inflammatory response, toxins from the traumatized area might run wild through the bloodstream and create a system-wide disturbance. Over the ensuing days, the inflammatory response helps these injuries heal by increasing blood flow to the affected areas, accelerating the removal of toxins, and repairing or regenerating damaged cells.
When inflammation-promoting environmental stimuli is chronic instead of acute, or occurs throughout the body instead of staying confined to the area of an acute injury, the inflammatory response becomes harmful. This is commonly described as chronic inflammation or systemic (system-wide) inflammation. For example, a high insulin-producing diet has a pro-inflammatory effect on the body. Consuming an excess of pro-inflammatory omega-6 fatty acids and insufficient amounts of anti-inflammatory omega-3 fatty acids also promotes systemic inflammation.
The condition of systemic inflammation results in excessive fluid retention in the cells. This can be reflected in bloating and puffy skin. Consequently, when dietary changes are made to achieve a better inflammatory balance, many experience less cellular fluid retention. This results in significant weight loss and noticeable changes in appearance in the initial weeks of diet modification. There is evidence to
Chronic exercise: Chronic exercise promotes systemic inflammation because the body’s stress response is overwhelmed by repeated demands on the natural, desirable inflammatory process that occurs in response to the stimulation of exercise. The acute inflammatory response to a workout is actually desirable, as muscles swell with blood and heat up to perform work efforts with maximum efficiency. The problem comes when the inflammatory response and stress response to exercise is called upon too frequently and/or with insufficient rest between challenging efforts. Such a chronic exercise pattern results in muscles, joints, and entire systems (cardiovascular system, immune system, endocrine system, etc.) becoming chronically inflamed. Without sufficient recovery time to restore and repair cells stressed by excessive workouts, injury, illness, and burnout are likely.
Inflammation and cancer: Many health and medical experts express the sentiment that inflammation is the root of all disease. Two key genes in the inflammatory process, cyclooxygenase-2 (COX-2) and nuclear factor-kappa B (NF-kappaB), provide a mechanistic link between inflammation and cancer. Inflammation induces these genes to inhibit apoptosis (desirable destruction of defective cells), stimulate angiogenesis (unhealthy cell division), and support cell proliferation. Chronically excessive levels of glucose and insulin in the bloodstream are leading causes of systemic inflammation.
Healthy gene expression is one of the primary goals of my Be Lean For Life Protocol. All 10 pillars work together to contribute to an optimal set of gene expressions for a lean and healthy life.
Essential Oils play a large role in Epigenetics

Hormonal: Aroma Touch, ClaryCalm, Clary Sage, Coriander, Eucalyptus, Jasmine, Magnolia, Myrrh, Star Anise, Yarrow Pom, Ylang Ylang, Yuzu, Zendricrine.
Note: Many different oils are listed above. While they are all relevant, nobody would ever use them all. If you are a Be Lean For Life Coaching client you may have the oils personally mapped to your specific requirement based on data collected during the coaching program.Paragraph
If you want to go it alone feel free to peruse the doTERRA Ebook Library. Alternatively, you can buy all these oils at wholesale prices by becoming a member


Recent Comments